Lactose Intolerance: Symptoms, Management, and Alternatives
Published:
Millions of people worldwide suffer from lactose intolerance, a digestive disorder that impairs the body's ability to break down milk sugar. This condition occurs when the body cannot properly digest lactose, the sugar found in milk and dairy products. In this guide, we will dive deep into the causes and effects of lactose intolerance, from exploring its biological basis to examining the symptoms it can cause.
Contents:
- Understanding Lactose Intolerance
- The Role of Lactase in Digestion
- Factors Causing Reduced Lactase Activity
- Understanding Lactose Intolerance
- The Role of Lactase in Digestion
- Factors Causing Reduced Lactase Activity
- Symptoms and Duration of Lactose Intolerance
- Diagnosing Lactose Intolerance
- Managing Symptoms through Dietary Adjustments
- Alternative Milk Options for Lactose Intolerance
- Probiotics for Gut Health in Lactose Intolerance
- Congenital Lactase Deficiency and Specialized Care
- FAQs in Relation to Lactose Intolerance
- Conclusion
From understanding the role of lactase enzyme in digestion to examining factors that cause reduced lactase activity, our discussion delves into the biological underpinnings of this condition. We'll also outline common symptoms experienced by those with lactose intolerance and discuss factors affecting their duration.
In addition to providing an overview of diagnostic methods such as hydrogen breath tests and stool acidity tests for identifying lactose intolerance, we will offer practical advice on managing symptoms through dietary adjustments. Furthermore, we will explore alternative milk options like almond milk and oat milk for those seeking dairy substitutes.
Lastly, our discussion covers probiotics' role in promoting gut health among individuals with lactase deficiency while highlighting congenital lactase deficiency's unique challenges requiring specialized care for infants affected by it.

Understanding Lactose Intolerance
This inability to digest lactose results from reduced levels of lactase activity, the enzyme responsible for breaking down lactose into simpler sugars that can be absorbed by the body.
The Role of Lactase in Digestion
Lactase is an essential enzyme produced in the small intestine, which plays a crucial role in breaking down lactose into glucose and galactose - two simple sugars that are easily absorbed by our bodies. When there is insufficient production or activity of this enzyme, undigested lactose remains within the digestive system, leading to various unpleasant symptoms associated with lactose intolerance.
Factors Causing Reduced Lactase Activity
- Genetics: Some individuals inherit genes that cause them to produce less active forms of the enzyme as they age. This type of genetic predisposition is known as lactase persistence/non-persistence.
- Gastrointestinal Disorders: Certain gastrointestinal conditions like celiac disease or Crohn's disease may lead to damage within the lining of your small intestine, resulting in decreased production/activity levels concerning enzymes required for proper digestion (including those needed for breaking down lactose).
- Small Intestinal Bacterial Overgrowth (SIBO): An imbalance of bacteria within the small intestine can cause reduced lactase activity, leading to symptoms similar to those experienced by individuals with lactose intolerance. Learn more about SIBO and its impact on digestion.
- Premature Birth: Infants born prematurely may have underdeveloped digestive systems that produce insufficient amounts of enzymes needed for proper digestion, including lactase. This condition is usually temporary as their digestive system matures.
In some cases, people may experience temporary lactose intolerance due to an illness or injury affecting their small intestine. Once the underlying issue has been resolved, normal levels of enzyme production/activity should resume - allowing them once again to consume dairy products without experiencing severe symptoms associated with this disorder.
Common symptoms of lactose intolerance include bloating, gas, abdominal pain, and diarrhea. If you suspect you may be lactose intolerant, lactose tolerance tests can help diagnose the condition. Treatment options include avoiding dairy products or consuming lactose-free milk and other lactose-free products.
It's important to note that lactose intolerance is not the same as a milk allergy. A milk allergy is an immune response to proteins found in milk, while lactose intolerance is a digestive disorder caused by the inability to digest lactose.
Understanding lactose intolerance and its symptoms can help individuals make informed decisions about their diet and lifestyle. By avoiding dairy products or consuming lactose-free alternatives, individuals with lactose intolerance can still enjoy a healthy and balanced diet.
Understanding Lactose Intolerance
This inability to digest lactose results from reduced levels of lactase activity, the enzyme responsible for breaking down lactose into simpler sugars that can be absorbed by the body.
The Role of Lactase in Digestion
When functioning properly, it breaks down this complex sugar into two simpler forms - glucose and galactose - allowing them to be easily absorbed by our bloodstream. However, individuals with lactose intolerance have insufficient amounts of this vital enzyme, leading to undigested lactose remaining within their digestive system.
Factors Causing Reduced Lactase Activity
- Genetics: Some people inherit genes associated with lower production or activity of the lactase enzyme from their parents. This genetic predisposition makes them more likely to develop lactase persistence or non-persistence.
- Ethnicity: Certain ethnic groups are more prone to developing this condition due to higher prevalence rates among their populations; examples include those of Asian, African, Native American, and Hispanic descent who tend towards having greater instances when compared against Caucasians living within similar geographical regions worldwide today (source).
- Gastrointestinal Disorders: Conditions such as celiac disease, Crohn's disease, and small intestinal bacterial overgrowth can damage the lining of the small intestine where lactase is produced. This may result in reduced lactase activity and subsequent lactose intolerance symptoms.
- Aging: As we age, our bodies naturally produce less lactase due to decreased enzyme production rates occurring over time - making it increasingly difficult for older adults, especially susceptible towards experiencing unpleasant symptoms associated with consuming dairy products containing high levels of this particular sugar compound (source).
In summary, various factors contribute to an individual's ability or inability to digest lactose effectively. Understanding these underlying causes can help inform appropriate treatment options and lifestyle adjustments necessary for managing this common yet often misunderstood condition more effectively moving forward into adulthood years ahead.
Understanding lactose intolerance is a complex condition that requires knowledge of the role of lactase in digestion and potential factors causing reduced activity. Now we can look into the indications and time frame of this ailment.
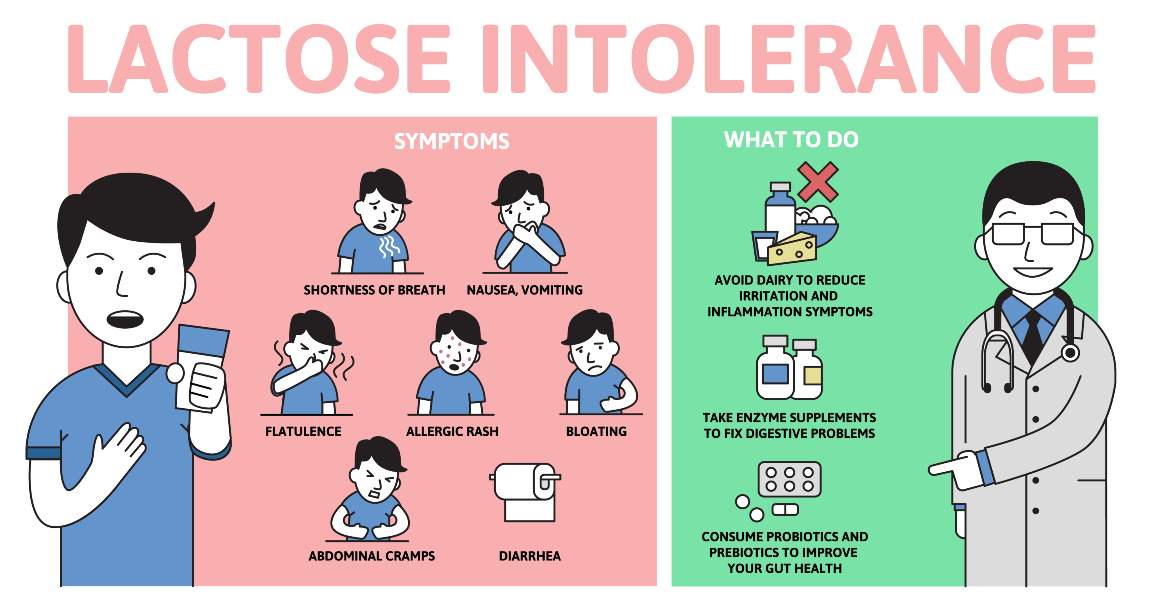
Symptoms and Duration of Lactose Intolerance
Lactose intolerance is a prevalent condition that many people experience globally. It occurs when the body cannot properly digest lactose, a sugar found in milk and dairy products. This inability to break down lactose leads to various gastrointestinal symptoms that can range from mild discomfort to severe pain.
Common Symptoms Experienced by Those with This Condition
The most common symptoms of lactose intolerance include:
- Bloating
- Gas
- Diarrhea
- Abdominal pain and cramps
- Nausea or vomiting (less common)
The presence of lactase, genetics, age and gut health can all influence the degree to which an individual experiences abdominal pain or cramps, nausea or vomiting due to lactose intolerance.
Factors Affecting Symptom Duration
The duration of lactose intolerance symptoms can also differ significantly between individuals. Generally speaking, these unpleasant effects may last anywhere from 30 minutes up to several hours after consuming foods containing lactase. Factors affecting symptom duration include:
- Dairy consumption frequency: Frequent consumption of dairy products may lead to more prolonged or severe symptoms due to increased exposure levels over time.
- Small intestinal bacterial overgrowth (SIBO): SIBO can cause similar symptoms to lactose intolerance and may exacerbate lactose intolerance symptoms.
- Other underlying conditions: Conditions such as celiac disease or Crohn's disease may cause similar symptoms to lactose intolerance and can make it difficult to diagnose the condition accurately.
- Amount of lactose consumed: The severity of symptoms may depend on the amount of lactose consumed. Small amounts of lactose may not cause any symptoms, while larger amounts may lead to more severe symptoms.
- Type of dairy product: Some dairy products, such as hard cheeses or lactose-free milk, may be better tolerated than others, such as ice cream or regular milk.
If you suspect that you may be lactose intolerant, it is recommended that you speak with your healthcare provider. They may recommend lactose tolerance tests or other diagnostic tests to determine if you have lactose intolerance. Additionally, there are many lactose-free milk and dairy products available that can help those with lactose intolerance enjoy the taste of milk products without experiencing unpleasant symptoms.
It is imperative to be cognizant of the indicators and period involved with lactose insensitivity in order to accurately diagnose this condition. The next heading will discuss two tests used for diagnosing lactose intolerance: a hydrogen breath test and stool acidity test.
Diagnosing Lactose Intolerance
Lactose intolerance can cause a variety of uncomfortable symptoms, making it essential to accurately diagnose the condition and rule out other potential causes for gastrointestinal distress like irritable bowel syndrome (IBS), celiac disease, or Crohn's disease. To do this, consult with your healthcare provider who will likely recommend testing methods such as hydrogen breath test or stool acidity test.
Hydrogen Breath Test Explained
The hydrogen breath test is a non-invasive diagnostic procedure that measures the amount of hydrogen in your breath after consuming a lactose-containing beverage. Since undigested lactose produces hydrogen gas when fermented by bacteria in the small intestine, elevated levels of hydrogen in your breath may indicate lactase deficiency and subsequent lactose intolerance.
- Preparation: Prior to the test, you'll need to follow specific dietary guidelines provided by your doctor to ensure accurate results.
- Procedure: On the day of the test, you'll drink a liquid containing lactose and then breathe into a device at regular intervals over several hours. The device measures hydrogen levels in your breath samples.
- Results interpretation: Your healthcare provider will analyze the collected data to determine if there's an increase in hydrogen production consistent with lactase deficiency and diagnose whether you have lactose intolerance or not.
Stool Acidity Test Overview
A stool acidity test is another diagnostic method that can be used, particularly for infants and young children who may not be able to undergo a hydrogen breath test. This test measures the amount of acid in stool samples, as undigested lactose produces lactic acid when fermented by bacteria in the small intestine.
- Preparation: Your healthcare provider will provide instructions on how to collect a stool sample from your child.
- Procedure: The collected sample is sent to a laboratory where it's analyzed for its acidity levels.
- Results interpretation: If high levels of lactic acid are detected in the stool sample, it may indicate lactase deficiency and suggest that your child has lactose intolerance.
Your doctor might also consider other factors, such as past medical records, relatives with lactose intolerance or dairy allergies, and dietary habits before coming to a definite diagnosis. Remember that only a qualified healthcare professional can diagnose this condition; self-diagnosis based on symptoms alone could lead to unnecessary dietary restrictions or overlooking other underlying health issues requiring treatment.
Accurately determining lactose intolerance is critical for effectively handling the condition. To ensure successful dietary adjustments, it's important to understand how to manage symptoms associated with lactose intolerance.
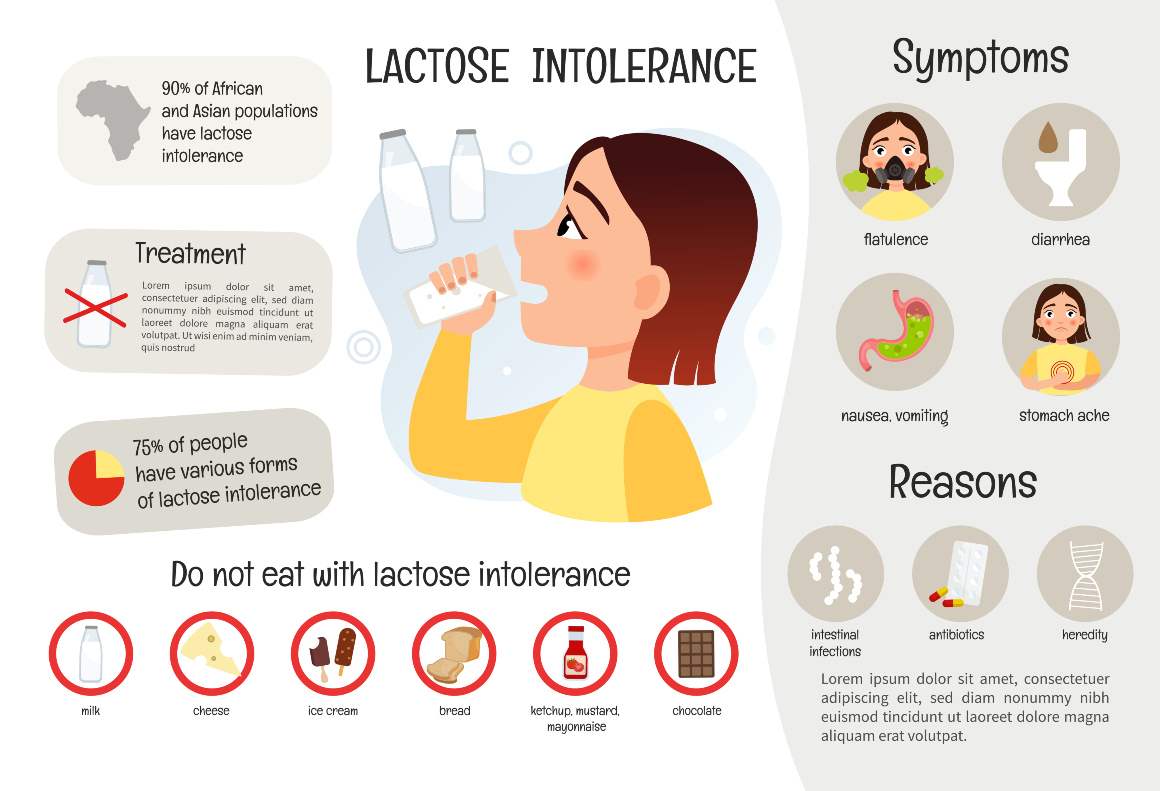
Managing Symptoms through Dietary Adjustments
Once diagnosed with lactose intolerance, managing its symptoms involves making dietary adjustments based on individual tolerance levels towards various foods containing varying amounts of natural or added sources of lactose content. This can help alleviate unpleasant symptoms and improve overall gut health.
Finding Your Lactose Tolerance Level
Eliminate all dairy from your diet for a brief span (normally 1-2 weeks) to figure out your lactose resilience level. Gradually reintroduce small amounts of different dairy products back into your diet while monitoring any potential reactions. Keep track of the types and quantities of dairy that trigger symptoms in order to establish which milk products you can tolerate without discomfort.
Dairy Alternatives for Lactose Intolerant Individuals
- Lactose-free milk: Many brands offer lactose-free cow's milk, which has been treated with the enzyme lactase to break down the lactose before consumption. This allows those who are intolerant to enjoy the taste and nutritional benefits of regular milk without experiencing digestive issues.
- Aged cheeses: Some aged cheeses like cheddar, Swiss, and Parmesan contain lower levels of lactose due to their longer fermentation process. These may be better tolerated by individuals with mild-to-moderate intolerance.
- Nondairy yogurts: Yogurt made from almond or coconut milk provides a lactose-free alternative for those who enjoy yogurt but cannot tolerate traditional dairy-based options. Look for brands that contain live and active cultures, as these can help support gut health.
- Ice cream substitutes: There are many dairy-free ice cream alternatives available made from almond milk, coconut milk, or soy milk. These can satisfy your sweet tooth without causing gastrointestinal distress associated with lactose intolerance.
Incorporating Lactase Supplements
If you still want to consume some dairy products despite being lactose intolerant, consider using over-the-counter lactase supplements. These supplements provide the enzyme needed to break down lactose in the small intestine and can be taken before consuming a meal containing dairy. However, it is important to consult with your healthcare provider before starting any new supplement regimen.
By making dietary adjustments, individuals with lactose intolerance can better manage their symptoms and live a healthier lifestyle. Furthermore, those with lactose intolerance can find suitable alternatives in milk substitutes such as almond or oat milk.
Alternative Milk Options for Lactose Intolerance
For those who cannot tolerate lactose, finding milk alternatives is essential to ensure that symptoms are not triggered. Some popular choices include almond milk, oat milk, and lactose-free cow's milk which can be consumed without triggering symptoms. This piece will discuss the potential advantages of lactose-free milk substitutes and how they can be used to keep up a nutritious eating regimen while evading undesirable indications.
Almond Milk Benefits for the Lactose Intolerant
Almond milk is a popular plant-based alternative to cow's milk made from almonds and water. It contains no lactose or dairy products, making it an ideal choice for individuals who are lactose intolerant. Almond milk also offers several health benefits such as:
- Low in calories compared to regular cow's milk.
- Naturally high in vitamin E which supports skin health.
- A good source of calcium when fortified - essential for strong bones and teeth.
- Dairy-free and vegan-friendly option suitable for various dietary preferences.
Oat Milk as a Dairy Substitute
Oat milk, another plant-based option gaining popularity among people with lactose intolerance, is made by blending oats with water then straining out the solids. This process results in a creamy liquid that resembles traditional cow's milk but does not contain any lactose or other problematic components for those with lactose intolerance. Some benefits of oat milk include:
- Rich in fiber, which promotes healthy digestion and can help manage symptoms associated with lactose intolerance.
- Naturally low in fat and cholesterol-free - beneficial for heart health.
- Fortified versions provide essential nutrients like calcium, vitamin D, and B vitamins.
In addition to almond and oat milk, there are other dairy alternatives available such as soy milk, rice milk, coconut milk, or even lactose-free cow's milk, specially formulated to remove the lactose content while retaining the taste and nutritional value of regular cow's milk. Experimenting with different options will help you find a suitable alternative that caters to your personal preferences without triggering any unpleasant symptoms due to lactose intolerance.
For those with lactose intolerance, alternative milk options can offer a nutritious and tasty substitute to dairy products. Moving on, probiotics are also important in aiding gut health when dealing with lactose intolerance.

Probiotics for Gut Health in Lactose Intolerance
Individuals with lactose intolerance can benefit from consuming probiotics-rich foods or supplements that contain live microorganisms known for promoting overall gut health by maintaining a healthy balance of intestinal flora. Incorporating these beneficial bacteria into one's diet can help alleviate some unpleasant symptoms associated with lactose intolerance and improve digestion.
The Role of Probiotics in Digestive Health
Probiotics are living organisms, primarily bacteria and yeasts, that provide numerous health benefits when consumed in adequate amounts. By promoting the activity of beneficial bacteria in the gut microbiome, probiotics can help to optimize digestive health. These friendly microbes aid in breaking down food particles, producing essential vitamins, and protecting against harmful pathogens.
In individuals with lactose intolerance, probiotics may assist in digesting undigested lactose by increasing levels of lactase activity. This helps reduce bloating, gas production, abdominal pain, and diarrhea often experienced after consuming dairy products containing lactose.
Best Probiotic Strains for Lactase Deficiency
Selecting appropriate probiotic strains is crucial to ensure optimal results when managing symptoms related to lactase deficiency. Some well-researched strains include:
- Lactobacillus acidophilus: A common strain found naturally within human intestines; it has been shown to produce its own form of lactase enzyme which aids in breaking down lactose.
- Bifidobacterium bifidum: This strain is known for its ability to improve overall gut health and has been found effective in alleviating symptoms of lactose intolerance by enhancing the digestion of dairy products.
- Lactobacillus bulgaricus: Often used as a starter culture in yogurt production, this probiotic strain can help break down lactose into simpler sugars that are more easily absorbed by the body.
To incorporate these beneficial strains into your diet, consider consuming foods like yogurt containing active cultures or taking high-quality probiotic supplements. Before beginning any new supplement program, it is essential to consult your healthcare provider - especially if you are experiencing severe symptoms or have an underlying medical condition like celiac disease or Crohn's.
For those with lactose intolerance, probiotics can be a helpful tool in maintaining digestive health; additionally, infants who may have congenital lactase deficiency require specialized care. By understanding the alternative feeding methods available, parents can ensure their infant receives adequate nutrition while managing any potential sensitivities.
Congenital Lactase Deficiency and Specialized Care
Congenital lactase deficiency is an extremely rare autosomal recessive disease characterized by absent or reduced enzymatic activity from birth. Children diagnosed with this condition require specialized care involving the use of alternative feeding methods and formulas designed specifically for their unique nutritional needs throughout infancy and early childhood stages. This ensures proper growth and development milestones are met without complications arising due to malnutrition resulting from inadequate intake or absorption capabilities when exposed solely to standard cow's milk-based infant formula options available commercially today.
Identifying Congenital Lactase Deficiency in Infants
Early diagnosis of congenital lactase deficiency is crucial for implementing appropriate dietary interventions that can prevent long-term health issues related to poor nutrient absorption. Some common symptoms associated with this condition include failure to thrive, diarrhea, vomiting, dehydration, and abdominal pain after consuming breast milk or conventional infant formulas containing lactose. If you suspect your child may have a congenital lactase deficiency, it is essential to consult with a pediatrician who will likely recommend diagnostic tests such as blood tests, stool acidity test, or genetic testing to confirm the diagnosis.
Alternative Feeding Methods and Formulas
Once a diagnosis has been made, healthcare providers will work closely with parents to develop an individualized feeding plan tailored specifically for infants suffering from congenital lactase deficiency. Some potential alternatives include:
- Lactose-free infant formulas: These specially formulated products contain all necessary nutrients required for healthy growth but exclude any sources of lactose found in traditional dairy-based options like cow's milk.
- Soy-based infant formulas: Made from soy protein isolate, these formulas are lactose-free and suitable for infants with a congenital lactase deficiency. However, it is essential to consult with your healthcare provider before using soy-based products as some children may have an allergy or intolerance to soy proteins.
- Hydrolyzed protein formulas: Also known as hypoallergenic formulas, hydrolyzed protein options break down proteins into smaller peptides that are easier for the digestive system to process. For infants with lactose intolerance and other food allergies/sensitivities, hydrolyzed protein formulas can be beneficial as they break down proteins into smaller peptides that are easier to digest.
In addition to alternative feeding methods and specialized infant formula options, parents should also work closely with their pediatrician or registered dietitian to ensure adequate nutrient intake through appropriate complementary foods once solid foods are introduced during weaning stages of development. As children grow older and transition into adolescence/adulthood phases where more diverse dietary choices become available - including various non-dairy milk alternatives like almond milk, oat milk, etcetera - maintaining proper nutrition remains paramount in order to prevent potential complications related directly or indirectly towards ongoing issues stemming from underlying congenital lactase deficiencies present since birth.
FAQs in Relation to Lactose Intolerance
What is the Latest Research on Lactose Intolerance?
Recent research on lactose intolerance focuses on genetic factors, improved diagnostic methods, and potential treatments. A significant study identified a single nucleotide polymorphism associated with lactase persistence/non-persistence in various populations. Other studies explore the efficacy of probiotics and enzyme replacement therapies to alleviate symptoms.
What are the Four Types of Lactose Intolerance?
The four types of lactose intolerance are:
- Congenital: caused by a genetic mutation that results in little or no production of lactase since birth.
- Primary: due to reduced production of lactase over time as part of the natural aging process.
- Secondary: a temporary condition resulting from an injury or illness affecting the small intestine.
- Dietary-induced: a rare form triggered by excessive consumption of dairy products leading to a temporary deficiency in producing sufficient amounts of lactase enzymes.
What is the Root Cause of Lactose Intolerance?
The root cause for most cases (primary) is a decrease in lactase enzyme production, which occurs naturally with age. Lactase breaks down milk sugar (lactose) into simpler sugars for absorption. In other cases, it may be due to congenital factors, secondary causes like gastrointestinal diseases or injuries, or dietary-induced reasons related to excessive dairy intake.
Conclusion
Hereditary factors or non-genetic causes can result in the inability to properly digest lactose, leading to uncomfortable symptoms such as bloating, gas and diarrhea. However, managing lactose intolerance through dietary changes and supplements can greatly improve digestion and prevent long-term health risks such as malnutrition and osteoporosis.
If you suspect that you may have lactose intolerance or are experiencing symptoms related to poor digestion of milk products, it's important to consult with a healthcare professional for proper diagnosis and treatment options. With the right approach, those who are lactose intolerant can still enjoy dairy products without suffering from unpleasant symptoms.
To support healthy digestion overall, consider incorporating probiotics into your daily routine. Cibdol offers high-quality probiotic supplements designed to promote gut health and boost immunity. Try them today!