Restless Leg Syndrome
Published:
Restless leg syndrome (RLS), also known as Willis-Ekbom disease, is a neurological disorder characterized by an irresistible urge to move one's legs accompanied by uncomfortable sensations. This condition can significantly impact sleep quality and overall well-being. In this guide, we will examine the characteristics of RLS, potential causes and risk factors associated with it, as well as strategies for managing symptoms during pregnancy.
Contents:
- Understanding Restless Leg Syndrome
- Common Symptoms of Restless Leg Syndrome
- How RLS Affects Sleep Quality
- Treatment Options for Restless Leg Syndrome
- Causes and Risk Factors of Restless Leg Syndrome
- Managing Restless Leg Syndrome During Pregnancy
- Treatment Options for Restless Leg Syndrome
- Role of Vitamins in Managing Restless Leg Syndrome
- Addressing Sleep-Related Issues in Restless Leg Syndrome Patients
- FAQs in Relation to Restless Leg Syndrome
- Conclusion
We will delve into the genetic factors contributing to RLS development and discuss underlying medical conditions linked with this disorder. Additionally, we'll examine how pregnant women can safely manage their restless legs symptoms during pregnancy.
Furthermore, our discussion on treatment options will cover both pharmacological interventions tailored according to patient-specific needs and non-pharmacological treatments like lifestyle modifications. We will also highlight the role of vitamins such as iron supplementation for RLS patients with iron deficiency and magnesium's role in reducing symptoms.
Last but not least, addressing sleep-related issues in restless leg syndrome patients is crucial; therefore, we'll help you understand the link between RLS and periodic limb movement disorder (PLMD) while providing strategies for improving sleep quality among those affected by this challenging condition.

Understanding Restless Leg Syndrome
Restless leg syndrome (RLS), also known as Willis-Ekbom disease, is a neurological movement disorder characterized by an uncontrollable urge to move the legs, often accompanied by uncomfortable sensations. This condition can make falling asleep and staying asleep difficult for many people, as they may feel the need to kick, squirm or massage their legs to lessen these sensations.
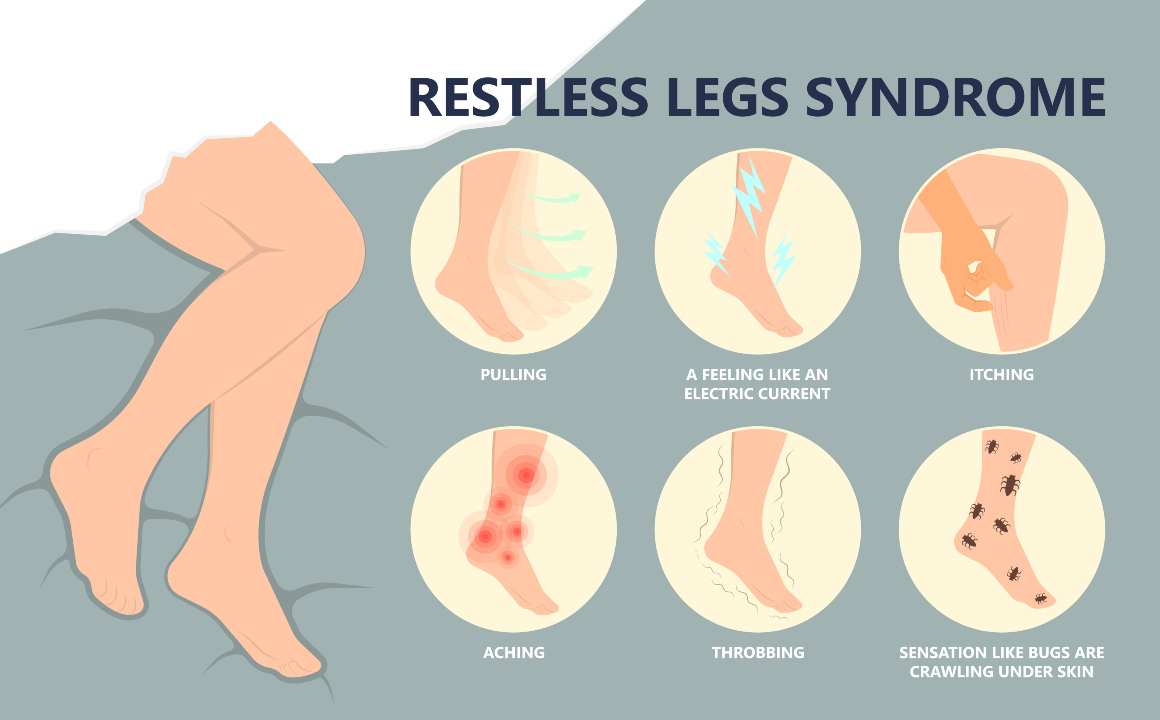
Common Symptoms of Restless Leg Syndrome
- An overwhelming urge to move the legs while at rest
- Sensations such as itching, burning, tingling or throbbing in the legs
- Movement providing temporary relief from symptoms
- Symptoms worsening during periods of relaxation or inactivity like bedtime
- Periodic limb movements during sleep (PLMS)
The severity of restless leg syndrome symptoms varies among individuals and can fluctuate throughout one's life. Some people experience mild discomfort occasionally, while others suffer from severe daily disturbances that significantly impact their quality of life.
How RLS Affects Sleep Quality
A major concern for those with restless leg syndrome is its negative effect on sleep quality. The constant need to move one's legs often leads to difficulty falling asleep and frequent awakenings throughout the night. Consequently, this results in daytime fatigue and impaired cognitive function due to insufficient restorative sleep.
In addition to the physical uneasiness that RLS can bring during slumber, it may also be responsible for insomnia or sleep apnea. These conditions further exacerbate the impact of restless leg syndrome on overall health and well-being.
Moreover, people with primary restless legs syndrome are more likely to experience mood disturbances like anxiety and depression due to their chronic sleep disturbance. This underscores the need for prompt diagnosis and proper management of this debilitating disorder.
Treatment Options for Restless Leg Syndrome
The initial treatment approach for managing symptoms includes non-pharmacological interventions such as lifestyle modifications (e.g., regular exercise, maintaining a consistent sleep schedule) and pneumatic compression devices that effectively treat patients with periodic limb movements during sleep (PLMS). However, if these measures do not provide adequate relief, pharmacological options may be considered.
- Dopamine agonists: Medications that increase dopamine levels in the brain have been shown to reduce symptoms in many cases of RLS. Examples include pramipexole and ropinirole.
- Iron supplementation: If an iron deficiency is identified as a contributing factor to RLS symptoms, oral iron supplements may be recommended under medical supervision.
- Gabapentin enacarbil: This medication has been approved by the FDA specifically for moderate-to-severe primary restless legs syndrome treatment due to its effectiveness in reducing uncomfortable sensations associated with the disorder.
In conclusion, restless leg syndrome is a debilitating condition that affects many people's quality of life. While there is no cure for RLS, appropriate management strategies can reduce symptoms and improve sleep quality. If you are experiencing restless leg symptoms, it is important to speak with your healthcare provider to determine the best course of action for you.
RLS can be a major impediment to getting adequate sleep, and should not be taken lightly. By understanding the causes and risk factors of RLS, we can begin to better understand how to manage this condition more effectively.
Causes and Risk Factors of Restless Leg Syndrome
Restless leg syndrome (RLS) is a complex neurological disorder with various contributing factors. The exact cause remains unknown, but researchers believe that it involves dopaminergic and brain iron dysregulation. Furthermore, certain genetic elements and medical issues may heighten the chance of developing RLS.
Genetic Factors Contributing to RLS Development
Six genes have been linked to a heightened likelihood of developing RLS, which are involved in dopamine regulation, nerve cell development and other nervous system-related processes. These genes are involved in dopamine regulation, nerve cell development, and other processes related to the nervous system. However, more genetic changes are likely to be discovered in the future as research continues on this topic. It's important to note that having these gene variants does not guarantee someone will develop RLS; rather, they simply increase their susceptibility.
Underlying Medical Conditions Linked with Restless Leg Syndrome
Besides genetics, several medical conditions may trigger or exacerbate restless leg syndrome symptoms. Some common examples include:
- Late-stage kidney disease: Patients undergoing dialysis often experience higher rates of RLS, possibly due to imbalances in electrolytes or toxins accumulating within the body.
- Iron deficiency: Low levels of iron can lead to insufficient dopamine production in the brain which might contribute towards restless legs symptoms. In fact, studies have shown that treating iron deficiency can help alleviate some cases of primary restless legs syndrome.
- Neuropathy: Nerve damage, particularly in the legs, can cause uncomfortable sensations and an urge to move that mimics RLS symptoms. This is especially common among individuals with diabetes or other conditions affecting nerve function.
- Multiple sclerosis (MS): People with MS are more likely to experience restless leg syndrome due to lesions within their central nervous system disrupting normal neurological processes.
- Parkinson's disease: Both Parkinson's disease and RLS involve dopamine dysregulation; therefore, it's not surprising that these two conditions often coexist. Researchers are still exploring the association between these two conditions.
In some cases, medications such as antidepressants or antipsychotics may also trigger restless legs symptoms. If you suspect your medication might be causing your RLS flare-ups, consult your healthcare provider for guidance on alternative treatment options.
Restless legs syndrome is often accompanied by periodic limb movements during sleep, which can cause sleep disturbance and lead to other sleep disorders. If you experience uncomfortable sensations in your legs that are relieved by movement, or if you have trouble sleeping due to leg movements, talk to your healthcare provider about potential treatment options. Dopamine agonists are a first-line treatment for RLS, but other medications and lifestyle changes may also help reduce symptoms.
Though the exact sources of RLS are not fully known, studies suggest that heredity and medical issues may be involved in its emergence. Given the higher incidence of RLS symptoms among pregnant women, it is essential to determine how to manage this condition in a safe manner during pregnancy.
Managing Restless Leg Syndrome During Pregnancy
Pregnant women experiencing this condition should consult their healthcare provider for appropriate management strategies on how to get rid of restless leg syndrome while pregnant without causing harm.
Prevalence of RLS in Pregnant Women
A study found that the prevalence of RLS among pregnant women ranges from 10% to 34%, with symptoms often worsening as the pregnancy progresses. The hormonal changes and increased iron requirements during pregnancy are believed to contribute to the development or exacerbation of RLS symptoms. Additionally, sleep disturbances caused by other factors such as physical discomfort or frequent urination can further aggravate restless legs symptoms in expectant mothers.
Safe Treatment Options During Pregnancy
Pregnancy poses unique challenges when it comes to treating restless leg syndrome, as some medications typically prescribed for RLS may not be safe for use during this time. Therefore, non-pharmacological approaches are usually recommended initially:
- Lifestyle modifications: Maintaining a regular sleep schedule, engaging in moderate exercise (with your doctor's approval), and practicing relaxation techniques like yoga or meditation can help alleviate RLS symptoms.
- Nutritional interventions: Ensuring adequate intake of essential nutrients like iron, magnesium, and folic acid through diet or supplements can help manage restless legs symptoms (source). Consulting with a medical professional before beginning any supplement routine is essential.
- Leg massages and warm baths: Massaging the legs or taking a warm bath before bedtime can help relax muscles and reduce discomfort associated with RLS.
In cases where non-pharmacological interventions are insufficient, some medications may be considered under close supervision by your healthcare provider. For example, low doses of dopamine agonists have been used in pregnant women with severe RLS symptoms (source). However, it is essential to weigh the potential benefits against any risks associated with medication use during pregnancy.
Managing restless leg syndrome during pregnancy requires careful consideration of both mother and baby's well-being. By working closely with their healthcare providers, expectant mothers can develop an individualized treatment plan that effectively addresses their symptoms while minimizing potential harm to their developing child.
By understanding the prevalence of RLS in pregnant women and implementing safe treatment options during pregnancy, we can help manage this condition. Various treatment options, tailored to the individual's requirements, exist for those enduring RLS - both pharmacological and non-pharmacological.
Treatment Options for Restless Leg Syndrome
Restless leg syndrome (RLS) can be a challenging condition to manage, but various treatment options are available. These treatments aim to reduce symptoms and improve sleep quality in affected individuals. Approaches include pharmacological interventions tailored according to patient-specific needs and non-pharmacological treatments like lifestyle modifications.
Pharmacological Interventions Tailored According to Patient-Specific Needs
The initial treatment for RLS often involves addressing any underlying conditions or factors contributing to the disorder, such as iron deficiency or neuropathy. In some cases, medication may be prescribed by healthcare providers depending on the severity of symptoms and individual patient needs. Some commonly used medications for managing RLS include:
- Dopamine agonists: Dopamine, believed to be involved in RLS, is increased by dopamine agonists.
- Alpha-2-delta ligands: Gabapentin and pregabalin are examples of this class of medications that help alleviate RLS symptoms by modulating calcium channels in nerve cells.
- Opioids: Low doses of opioids such as tramadol or oxycodone may be prescribed when other treatments have not been effective at controlling severe RLS symptoms.
- Benzodiazepines: Clonazepam, a benzodiazepine, may be prescribed to assist with sleep disturbances caused by PLMS (Periodic Limb Movements during Sleep), which is frequently seen in conjunction with RLS.
Before taking any medication for RLS, it is important to consult a healthcare provider as certain drugs may have adverse effects or interact with other medications.
Non-Pharmacological Treatments Like Lifestyle Modifications
In addition to pharmacological interventions, several non-medicinal approaches can help manage restless leg syndrome symptoms. Some of these include:
- Lifestyle changes: Regular exercise, maintaining a consistent sleep schedule, and avoiding caffeine and alcohol close to bedtime may help reduce RLS symptoms.
- Leg massages: Massaging the legs can provide temporary relief from uncomfortable sensations associated with restless legs syndrome.
- Warm baths: Soaking in warm water before bed may help relax muscles and alleviate RLS-related discomfort.
Pneumatic compression devices are another non-pharmacological treatment option that has been found effective in treating patients with periodic limb movements during sleep (PLMS), which often coexist with restless legs syndrome. These devices apply pressure to the limbs through inflatable cuffs wrapped around them, promoting blood flow and reducing PLMS episodes.
Treating restless leg syndrome requires a comprehensive approach considering individual patient needs and preferences. By collaborating with medical professionals, individuals can identify a suitable blend of interventions that efficiently regulate their indications while minimizing possible side effects or drug interactions.
Tailoring treatment for RLS to the individual's needs may involve pharmacological or non-pharmacologic strategies. Moving on, it is important to consider the role of vitamins in managing RLS symptoms as well.
Role of Vitamins in Managing Restless Leg Syndrome
While various treatment options are available, some vitamins have been found to help manage RLS symptoms effectively. Before beginning any vitamin supplementation regimen, it is important to consult with a healthcare provider.
Iron Supplementation for RLS Patients with Iron Deficiency
Research has shown that iron deficiency may contribute to the development or worsening of restless legs syndrome. For patients with iron deficiency, supplementation may be advised to address RLS symptoms, and dietary intake of iron-rich foods can also help boost natural levels. Oral iron supplements are typically prescribed; however, intravenous administration might be necessary in severe cases or when oral absorption is compromised.
- Increasing dietary iron intake with foods such as red meat, poultry, fish, beans and leafy greens can help to naturally raise levels.
- Maintain proper dosage: Always follow your healthcare provider's recommendations regarding supplement dosages and duration.
- Monitor progress: Regular blood tests should be conducted to ensure appropriate levels are maintained and adjust the treatment plan accordingly if needed.
Magnesium's Role in Reducing RLS Symptoms
Magnesium plays an essential role in regulating muscle function and nervous system activity. Some studies suggest that magnesium deficiency could exacerbate restless legs symptoms due to its involvement in neurotransmitter production - specifically dopamine - which has been linked with RLS pathophysiology (source). Healthcare professionals may suggest magnesium supplementation as a potential treatment for RLS, though further research is necessary to validate this idea.
- Choose the right form: Magnesium supplements come in various forms such as magnesium citrate, oxide and glycinate. Consult your healthcare provider to determine which type is best suited for you.
- Monitor dosage: Excessive intake of magnesium can lead to side effects like diarrhea or stomach cramps. Always follow the recommended dosages provided by your healthcare professional.
In addition to iron and magnesium, other vitamins and minerals have been suggested as potential treatment options for restless leg syndrome. For example, vitamin D deficiency has been linked with increased RLS symptoms (source). However, further research is necessary before establishing a definitive connection between specific nutrient deficiencies and restless legs syndrome development or progression.
It's crucial not only to address any underlying nutritional deficiencies but also consider lifestyle modifications that could help alleviate symptoms of this condition. Regular exercise, maintaining a consistent sleep schedule, and avoiding caffeine are just a few examples of non-pharmacological interventions that can be beneficial in managing restless leg syndrome alongside appropriate vitamin supplementation when required.
Vitamins can be a factor in managing restless leg syndrome, yet other sleep-related matters must be taken into account for the most desirable result. Therefore, it is necessary to understand the link between RLS and PLMD as well as implement strategies for improving sleep quality in RLS patients.

Addressing Sleep-Related Issues in Restless Leg Syndrome Patients
Most people with restless leg syndrome also suffer from periodic limb movement disorder (PLMD), a condition involving repetitive flexing or twitching of limbs during nighttime sleep. This highlights the need for comprehensive treatment plans targeting both disorders concurrently to achieve optimal therapeutic outcomes among affected individuals.
Understanding the Link Between RLS and PLMD
Studies have shown that up to 80% of patients with restless legs syndrome also experience periodic limb movements, which can further disrupt their sleep quality. These involuntary movements typically occur every 20-40 seconds throughout the night and are characterized by brief muscle contractions in the lower extremities. The exact cause behind this association between RLS and PLMD remains unclear; however, researchers believe that common underlying factors such as dopamine dysregulation or iron deficiency may contribute to both conditions.
Strategies for Improving Sleep Quality in RLS Patients
To address sleep disturbances associated with restless leg syndrome and periodic limb movement disorder, healthcare providers often recommend a combination of pharmacological treatments and lifestyle modifications:
- Dopamine agonists: Medications like pramipexole, ropinirole, or rotigotine can help regulate dopamine levels within the central nervous system, reducing symptoms of both RLS and PLMD.
- Sleep hygiene practices: Establishing a consistent bedtime routine, creating a comfortable sleeping environment free from distractions, avoiding caffeine close to bedtime, and engaging in relaxation techniques before sleep can help improve overall sleep quality.
- Exercise: Regular physical activity has been shown to reduce symptoms of restless legs syndrome and may also contribute to better sleep. However, it is essential not to exercise too close to bedtime as this can exacerbate RLS symptoms.
- Pneumatic compression devices: These devices apply pressure on the lower limbs during sleep, which can help reduce periodic limb movements and improve sleep quality in some patients with PLMD.
In addition to these strategies, healthcare providers may recommend other treatments based on individual patient needs. For example, if iron deficiency is identified as a contributing factor for both RLS and PLMD, supplementation with iron may be prescribed under medical supervision. Similarly, medications like benzodiazepines or anticonvulsants might be considered for specific cases where dopamine agonists are contraindicated or insufficiently effective.
Treating restless leg syndrome and periodic limb movement disorder concurrently requires a comprehensive approach that addresses the underlying causes while improving sleep quality. By working closely with their healthcare provider, individuals affected by these conditions can develop tailored treatment plans that effectively manage their symptoms and promote restful nights of sleep.
FAQs in Relation to Restless Leg Syndrome
What is the Latest Research on Restless Leg Syndrome?
New research on restless leg syndrome focuses on understanding its genetic basis, exploring potential treatments, and identifying possible links with other sleep disorders. Recent studies have discovered overlapping risk genes between insomnia and restless leg syndrome, which may help in developing targeted therapies for both conditions.
What is the Number One Cause of Restless Leg Syndrome?
The exact cause of restless leg syndrome remains unknown; however, it is believed to be a combination of genetic factors and underlying medical conditions such as iron deficiency or peripheral neuropathy. In some cases, pregnancy can also trigger restless leg syndrome symptoms temporarily.
What Stops Restless Leg Syndrome Immediately?
To alleviate restless leg syndrome symptoms immediately, try massaging your legs, applying warm or cold packs to affected areas, engaging in moderate exercise like walking or stretching before bedtime. Additionally, maintaining good sleep hygiene, and avoiding caffeine and alcohol close to bedtime can help reduce symptom severity.
What are the Roots of Restless Legs?
The roots of restless leg syndrome are not entirely understood but involve a complex interplay between genetics and environmental factors. Studies suggest that there might be an imbalance in dopamine levels within the brain affecting muscle movements while others point towards issues related to iron metabolism. Underlying medical conditions may also contribute to restless leg syndrome development.
Conclusion
Restless leg syndrome is a neurological disorder that affects sleep quality and causes an uncontrollable urge to move the legs. It can be caused by genetic factors or underlying medical conditions. Safe treatment options are required for managing it during pregnancy. Treatment options for RLS include pharmacological interventions tailored according to patient-specific needs and non-pharmacological treatments like lifestyle modifications.
Iron supplementation is an important consideration for RLS patients with iron deficiency, and magnesium may also help reduce RLS symptoms. Addressing sleep-related issues in RLS patients involves understanding the link between RLS and periodic limb movements, as well as strategies for improving sleep quality.