Insomnia Treatment : Guide to Better Sleep
Published:
Tackling insomnia necessitates a comprehensive approach that involves knowledge of the diverse forms and their root causes. This blog post will delve into the different classifications of insomnia, ranging from acute to chronic forms, as well as primary and secondary cases.
Contents:
- Types of Insomnia
- Non-pharmacological Interventions for Insomnia Treatment
- Pharmacologic Treatment Options for Insomnia
- Specific Drugs Marketed for Treating Insomnia
- Alternative Therapies and Off-Label Use of Medications
- Specific Drugs Marketed for Treating Insomnia
- Alternative Therapies and Off-Label Use of Medications
- Insomnia Treatment In Older Adults
- Acupressure as a Complementary Therapy for Insomnia
- FAQs in Relation to Insomnia Treatment
- Conclusion
We will explore non-pharmacological interventions for treating insomnia, including counseling techniques for managing stressors affecting sleep patterns, cognitive-behavioral therapy methods targeting negative thought processes, and sleep hygiene education promoting healthy lifestyle habits.
Furthermore, we'll discuss pharmacologic treatments for insomnia such as orexin receptor antagonists like Suvorexant and Daridorexant, melatonin receptor agonists such as Ramelteon. We will also compare the efficacy of melatonin supplements versus agonists in treating insomnia symptoms.
In addition to these approaches to insomnia treatment, we'll address unique challenges faced by older adults due to cognitive decline and hormonal changes. Lastly, this post will introduce acupressure therapy as an alternative method for treating insomnia while discussing its long-term benefits when incorporated into a holistic treatment plan.

Types of Insomnia
Insomnia can be classified into various types, each with its unique characteristics and potential causes. Understanding the type of insomnia is crucial for determining the most effective treatment approach. In this section, we will discuss acute, transient, chronic, primary, and secondary insomnia.
Acute Insomnia
Short-term insomnia, or adjustment sleep disorder, typically lasts a few days to weeks and is usually resolved when the triggering event has passed. It often results from stressors such as work-related issues or significant life events like losing a loved one. Acute insomnia usually resolves on its own once the triggering event has passed.
Transient Insomnia
Transient insomnia is temporary in nature and lasts less than a week. This form of difficulty falling asleep may be caused by factors such as jet lag or changes in sleeping environment. Like acute insomnia, it generally resolves without intervention once the underlying cause is addressed.
Chronic Insomnia
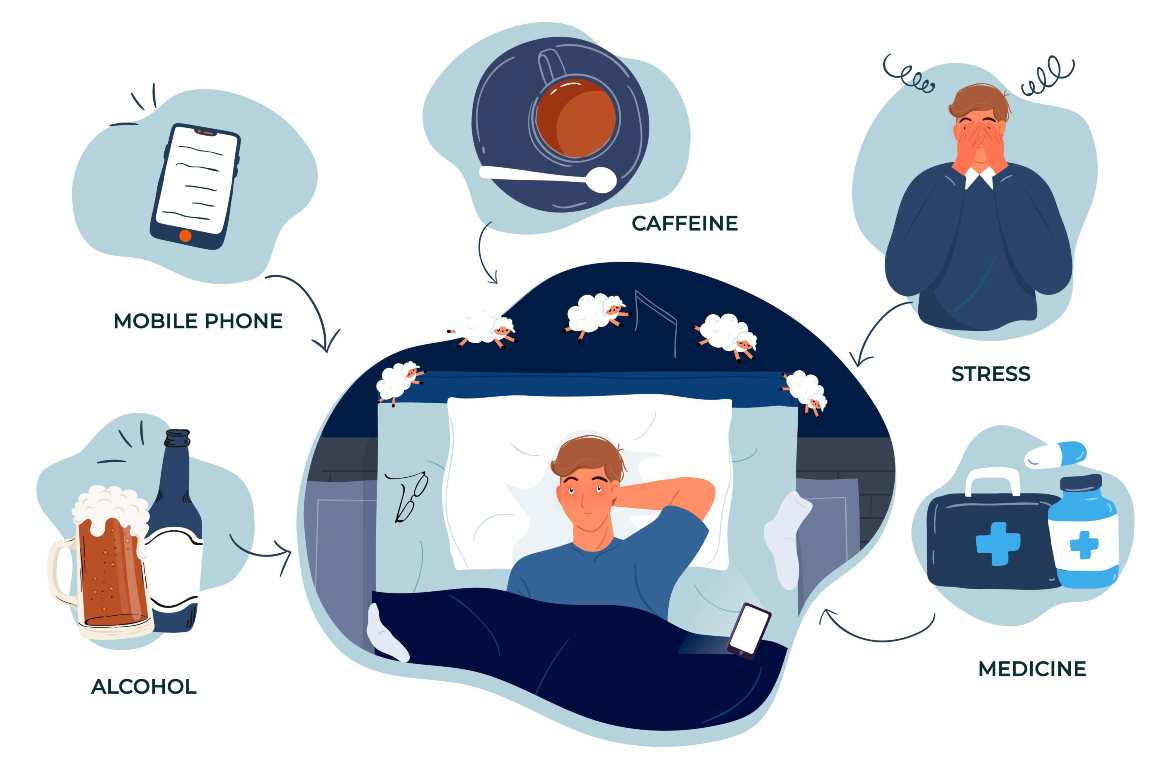
Chronic insomnia, on the other hand, is characterized by disrupted sleep that occurs at least three nights per week for at least three months. It can result from an array of factors including medical conditions (e.g., sleep apnea), medication side effects, lifestyle habits (e.g., caffeine consumption), and mental health disorders (e.g., anxiety). Treating chronic insomnia often requires a combination of pharmacological and non-pharmacological interventions such as relaxation techniques, cognitive-behavioral therapy, and drug administration.
Primary Insomnia
Primary insomnia is not associated with another condition or disorder. It may be caused by genetic factors, poor sleep habits, or an overactive arousal system. Treatment for primary insomnia typically focuses on improving sleep hygiene and addressing any underlying behavioral issues that contribute to the problem.
Secondary Insomnia
In contrast, secondary insomnia results from an underlying cause such as medical conditions (e.g., restless legs syndrome), medication side effects, or substance use disorders. Addressing the root cause of secondary insomnia is essential for effective treatment.
In summary, identifying the type of insomnia experienced can help guide appropriate treatment strategies to improve sleep quality and alleviate daytime symptoms like difficulty concentrating and fatigue.
Sleep disruption, a widespread problem, can have many triggers and it is vital to comprehend the different kinds of insomnia in order to adequately treat it. To further explore treatment options for insomnia, non-pharmacological interventions should also be considered.
Non-pharmacological Interventions for Insomnia Treatment
Non-pharmacological interventions play a significant role in treating insomnia, as they address thoughts and behaviors that contribute to poor sleep habits while promoting relaxation techniques and establishing healthy bedtime routines. These approaches are often recommended before resorting to medications, as they carry fewer side effects and can be more sustainable long-term solutions.
Cognitive-behavioral therapy for chronic insomniacs
CBT is the preferred treatment for individuals suffering from chronic insomnia, as it works to replace negative thought patterns related to sleep with positive ones. CBT focuses on identifying negative thought patterns related to sleep, such as anxiety about falling asleep or staying asleep, which may exacerbate the difficulty of sleeping. Through various exercises and strategies like stimulus control, sleep restriction, and relaxation training, patients learn how to change these unhelpful thoughts into more positive ones that promote better sleep quality.
Sleep hygiene education tips
Educating oneself about proper sleep hygiene is another essential component of non-pharmacological treatments for insomnia. Sleep hygiene refers to habits and practices that improve nighttime restfulness while minimizing daytime sleepiness. Some effective tips include:
- Maintaining a consistent bedtime routine: Going to bed at the same time every night helps regulate your body's internal clock.
- Avoiding stimulants close to bedtime: Consuming caffeine or nicotine can disrupt sleep onset by increasing alertness levels.
- Cultivating a relaxing bedroom environment: A comfortable mattress, dark curtains, and a cool room temperature can help facilitate falling asleep.
- Limiting screen time before bed: Exposure to blue light from electronic devices can interfere with the production of melatonin, making it more difficult to fall asleep.
- Incorporating relaxation techniques into your bedtime routine: Deep breathing exercises, progressive muscle relaxation, or meditation can help calm the mind and body in preparation for sleep.
Cognitive-behavioral therapy combined with instruction in proper sleep practices may lead to substantial enhancements in an individual's ability to drift off and stay asleep during the night. These non-pharmacological interventions offer a safer alternative to medications while addressing the root causes of disrupted sleep patterns.
Non-medicinal strategies for managing insomnia can offer aid from the signs of persistent sleeplessness, but in more serious cases medication treatments might be essential. Therefore, it is important to explore all available options when considering a course of action for treating insomnia.

Pharmacologic Treatment Options for Insomnia
Hypnotic medications have proven to be efficacious for the short-term treatment of different forms of insomnia. Sedative-hypnotic drugs are commonly prescribed today due to their lower side effects profile compared to antidepressants, which were once widely used but are now avoided because they carry more risks.
FDA-Approved Hypnotic Medications
The Food and Drug Administration (FDA) has approved several sleeping pills that help people with insomnia fall asleep, stay asleep, or both. These medications include benzodiazepines like temazepam and non-benzodiazepine hypnotics such as zolpidem, eszopiclone, and zaleplon. While these drugs can be effective in treating insomnia symptoms, it is essential to use them under a doctor's supervision due to the potential for dependence and other side effects.
Melatonin Receptor Agonists like Ramelteon
Melatonin receptor agonists, such as ramelteon, are another class of FDA-approved sleep aids that work by targeting melatonin receptors in the brain responsible for regulating sleep-wake cycles. Unlike sedative-hypnotics, melatonin receptor agonists do not have sedative effects or pose a risk of dependency. However, their efficacy may vary depending on individual factors such as age and underlying medical conditions.
Specific Drugs Marketed for Treating Insomnia
Several classes of drugs have been approved by the FDA specifically targeting different aspects related to pathways involved in regulating normal sleeping patterns. Orexin receptor antagonists like Suvorexant and Daridorexant are examples. These medications improve sleep quality, particularly among those with severe or chronic cases.
Orexin Receptor Antagonists: Suvorexant & Daridorexant
Orexin receptor antagonists such as suvorexant and daridorexant work by blocking the action of orexin, a neurotransmitter that promotes wakefulness. By inhibiting this neurotransmitter, these drugs help individuals with insomnia fall asleep faster and stay asleep longer. Side effects of orexin receptor antagonists, such as suvorexant and daridorexant, may include daytime sleepiness and difficulty focusing.

Alternative Therapies and Off-Label Use of Medications
Ramelteon, an off-label melatonin agonist, may offer some benefit in treating insomnia symptoms, although the efficacy of long-term use is uncertain. However, off-label use of melatonin agonists like ramelteon has demonstrated some promise in treating insomnia symptoms.
Off-Label Use of Ramelteon
Ramelteon is primarily prescribed for sleep onset difficulties, but its off-label use has shown potential benefits for other types of insomnia as well. As an alternative to traditional hypnotics or sedatives, ramelteon offers fewer risks related to dependency or adverse reactions while still providing relief from difficulty falling asleep.
Pharmacologic Treatments Options for Insomnia are a viable option to treat insomnia, however it is important to discuss these treatments with your doctor before taking any medications. Moving on from this, the next heading focuses specifically on drugs marketed for treating insomnia such as Orexin Receptor Antagonists.
Specific Drugs Marketed for Treating Insomnia
In recent years, the development of new medications has led to a variety of drugs specifically designed for treating insomnia. These medications target different aspects and pathways involved in regulating normal sleeping patterns, offering improved sleep quality for those with severe or chronic cases.
Orexin Receptor Antagonists: Suvorexant & Daridorexant
Orexin receptor antagonists, such as Suvorexant and Daridorexant, are examples of innovative treatments that have been approved by the Food and Drug Administration (FDA) for insomnia treatment. Orexin is a neurotransmitter responsible for promoting wakefulness; thus, blocking its action can help individuals fall asleep more easily.
- Suvorexant: This drug was the first orexin antagonist approved by the FDA in 2014. Suvorexant targets both orexin-A and orexin-B receptors in the brain's lateral hypothalamus region to regulate sleep-wake cycles. Clinical trials have demonstrated suvorexant's effectiveness in reducing sleep onset latency (time taken to fall asleep) and increasing total sleep time among adults with primary insomnia (source). However, it should be noted that some patients may experience side effects like daytime drowsiness or abnormal dreams.
- Daridorexant: A newer addition to this class of drugs is daridorexant, which was approved by the FDA in 2023. It has shown promising results in clinical trials for treating insomnia, with participants reporting improvements in sleep onset latency and wake after sleep onset (source). Daridorexant is considered to have a favorable safety profile compared to other hypnotic medications due to its lower risk of next-day residual effects.
It's important to note that while these drugs are specifically marketed for insomnia treatment, they may not be suitable for everyone. Patients should speak to their healthcare provider prior to beginning any medication regimen and consider potential adverse effects or drug interactions.
In addition to orexin receptor antagonists, there are also other classes of drugs available for treating insomnia symptoms such as benzodiazepines (e.g., temazepam), non-benzodiazepine hypnotics (e.g., zolpidem), and melatonin receptor agonists (e.g., ramelteon). However, each class comes with its own set of risks and benefits that must be carefully weighed against individual patient needs/preferences based on severity/type underlying causes related comorbidities if present (e.g., anxiety/depression).
The Orexin Receptor Antagonists Suvorexant and Daridorexant are two drugs that have been specifically marketed for treating insomnia. Still, other approaches to managing insomnia might be looked at, such as alternative therapies or utilizing drugs for purposes not specified in their labeling.

Alternative Therapies and Off-Label Use of Medications
While melatonin supplements are widely available and often used for sleep issues, they are not recommended as a first-line treatment option due to limited evidence supporting their efficacy and concerns about potential side effects associated with long-term use. However, off-label use of certain medications has demonstrated some promise in treating insomnia symptoms.
Off-Label Use of Ramelteon
Ramelteon, a melatonin receptor agonist, is one such medication that has shown effectiveness in improving sleep quality when used off-label for insomnia treatment. This medication works by replicating the impacts of melatonin in the body, thus helping to keep up a regular sleep-wake cycle and encouraging undisturbed rest without inducing any drowsiness or sedative effects which are usually observed with traditional sleeping medications.
Ramelteon is approved by the Food and Drug Administration (FDA) for treating difficulty falling asleep but not specifically marketed for chronic insomnia treatment. Despite this limitation, studies have found it to be effective in reducing nighttime awakenings and increasing total sleep time among individuals struggling with various forms of insomnia including transient, short-term, and chronic cases.
- Efficacy: Research suggests that ramelteon can improve both subjective measures like self-reported satisfaction with sleep quality as well as objective markers such as reduced latency to persistent sleep compared to placebo groups.
- Safety Profile: Unlike many hypnotic medications which carry risks related to dependency and withdrawal symptoms, ramelteon has a favorable safety profile with minimal risk of abuse or addiction. Additionally, it does not appear to impair next-day cognitive functioning or cause residual sedation.
- Comorbidities: Ramelteon may be particularly beneficial for individuals who have difficulty falling asleep due to co-occurring conditions such as anxiety disorders, depression, and chronic pain that disrupts sleep onset.
More research is necessary to ascertain the long-term efficacy and safety of ramelteon when used off-label for insomnia. It is essential for anyone looking into utilizing any medication to help with insomnia - be it on- or off-label - to confer with their medical provider regarding the possible advantages and hazards connected with each choice prior to settling on a conclusion.
The off-label use of medications can be an effective alternative to traditional insomnia treatments, but it is important to consider the age and other factors that may influence sleep quality when determining the best course of action. Tailoring treatments for older adults should be a priority in order to ensure optimal results from any therapy or medication prescribed.
Insomnia Treatment In Older Adults
Older adults may experience unique challenges due to cognitive decline and hormonal changes impacting normal sleeping patterns. The best approach for managing insomnia involves a combination of non-pharmacological strategies such as cognitive-behavioral therapy (CBT), sleep hygiene education alongside targeted pharmacotherapy options tailored according to individual patient needs/preferences based on severity/type underlying causes related comorbidities if present (e.g., anxiety/depression).
Tailoring Treatments for Older Adults
In order to effectively treat insomnia in older adults, it is essential to consider the specific factors that contribute to their difficulty sleeping. For example, age-related conditions like sleep apnea or restless legs syndrome can disrupt sleep and require specialized treatment approaches. Additionally, medications commonly prescribed for other health issues might have sedative effects or cause daytime sleepiness, further complicating the management of insomnia.
- Cognitive-Behavioral Therapy: CBT has been proven effective in treating chronic insomnia by addressing thoughts and behaviors that contribute to poor sleep habits while promoting relaxation techniques and establishing healthy bedtime routines.
- Sleep Hygiene Education: Educating older adults about proper sleep hygiene practices can help improve their overall quality of life by encouraging good habits such as maintaining a consistent bedtime schedule, creating a comfortable sleeping environment, limiting caffeine intake before bed, etc.
- Pharmacologic Interventions: When necessary, targeted pharmacotherapy options should be considered, taking into account the patient's medical history and potential interactions with other medications they may be taking. It is crucial to consult a healthcare professional before starting any new medication for insomnia.
Addressing Age-Related Factors Affecting Sleep Quality
Beyond tailored treatment approaches, it is essential to address age-related factors that can negatively impact sleep quality in older adults. For instance, menopause can cause hormonal changes leading to difficulty falling asleep or staying asleep. Similarly, chronic pain from conditions like arthritis or neuropathy might disrupt sleep patterns.
To improve sleep quality among older adults experiencing these challenges:
- Encourage regular physical activity during the day to promote better nighttime rest.
- Recommend relaxation techniques such as deep breathing exercises or meditation practices that can help reduce stress and anxiety levels before bedtime.
- Suggest using assistive devices (e.g., pillows designed for specific sleeping positions) or pain management strategies (e.g., heat therapy) when necessary to alleviate discomfort while resting.
Incorporating non-pharmacological approaches, in combination with appropriate drug management, can drastically improve the results of treating insomnia in seniors, and ultimately raise their overall health and satisfaction.
In summary, when managing insomnia in seniors, a personalized approach should be taken into account to take into consideration any age-related factors that could affect sleep. Moving on, acupressure can be used as a complementary therapy for treating insomnia and improving sleep quality.
Acupressure as a Complementary Therapy for Insomnia
Sleep disruption is a common issue that plagues countless individuals around the world. While medications and other treatments can help manage the symptoms, many individuals are seeking alternative or complementary therapies to improve their sleep quality without relying solely on pharmaceuticals. An alternative therapy for managing insomnia that has gained traction is acupressure.
Benefits of Acupressure in Improving Sleep Quality
A recent longitudinal study by Sun et al. found that consistent acupressure treatment could significantly improve insomnia symptoms over time. This non-invasive therapy offers several benefits for those struggling with chronic insomnia, difficulty falling asleep, staying asleep, or experiencing daytime sleepiness due to disrupted sleep patterns:
- Natural approach: Acupressure relies on the body's natural healing abilities rather than introducing external substances like sleeping pills or sedative effects from medications.
- No side effects: Unlike some pharmacological interventions used to treat insomnia, acupressure does not have any known adverse side effects when performed correctly.
- Ease of use: Individuals can learn simple techniques and apply them at home using their fingers or specialized tools designed for this purpose (e.g., an acupressure mat).
- Holistic benefits: In addition to improving sleep quality, regular acupressure sessions may also provide relief from related issues such as anxiety, depression, and chronic pain which often coexist with sleep disorders like restless legs syndrome and obstructive sleep apnea.
To maximize the potential benefits of acupressure for insomnia treatment, it is essential to target specific pressure points known to influence sleep onset and quality. Some commonly used acupressure points include:
- Anmian (Peaceful Sleep): Located behind the earlobe, this point is believed to promote relaxation and induce sleep.
- Shenmen (Spirit Gate): Found on the inner wrist crease, applying pressure here may help calm the mind and alleviate anxiety that disrupts sleep.
- Yin Tang (Hall of Impression): Situated between the eyebrows, stimulating this area can encourage a sense of tranquility conducive to falling asleep more easily.
Integrating acupressure with cognitive-behavioral therapy, relaxation techniques and other non-pharmacological interventions may offer a comprehensive approach to treating chronic insomnia. However, it's crucial to consult with a healthcare professional before starting any new treatment regimen, especially if you have pre-existing medical conditions or are currently taking medications for insomnia or other sleep disorders.
FAQs in Relation to Insomnia Treatment
What is the most successful treatment for insomnia?
The most successful treatment for insomnia often involves a combination of cognitive-behavioral therapy (CBT) and sleep hygiene education. CBT targets negative thought processes, while sleep hygiene promotes healthy lifestyle habits to improve sleep quality. In some cases, pharmacologic treatments like melatonin receptor agonists or orexin receptor antagonists may be prescribed as well.
What is a good treatment for insomnia?
A good treatment for insomnia includes non-pharmacological interventions such as counseling techniques to manage stressors affecting sleep patterns, cognitive-behavioral therapy methods targeting negative thoughts, and sleep hygiene education. Pharmacologic treatments like melatonin supplements or prescription medications can also be effective when used appropriately under medical supervision.
What is the scholarly treatment for insomnia?
Scholarly treatments for insomnia are evidence-based approaches supported by scientific research. These include cognitive-behavioral therapy, which has been proven effective in treating both acute and chronic forms of the condition, and pharmacologic options such as orexin receptor antagonists or melatonin receptor agonists that have undergone rigorous clinical trials to ensure their safety and efficacy.
Conclusion
In conclusion, insomnia can take many forms and have various underlying causes. Non-medicinal methods, like talking therapy, cognitive-behavioral treatment and guidance on how to improve sleep hygiene can be successful in managing insomnia symptoms. Pharmacologic treatments such as orexin receptor antagonists and melatonin receptor agonists can also be used to manage the condition. Older adults face unique challenges when it comes to managing their insomnia due to cognitive decline and hormonal changes.
Acupressure is a holistic alternative treatment that has shown promise in improving sleep quality over time. Overall, there are multiple options available for those seeking help with their insomnia treatment.








